It can be confusing to determine whether you have binge eating, food addiction or emotional eating. While criteria for binge eating disorder have been established for some time, research is beginning to show some of the ways in which binge eating and food addiction are similar and different. All of these disorders can affect men as well as women and are related to how you use food. It’s not food or your body that is the problem, it has to do with how you use food that may stem from early life adversity, trauma or neglect.
In this podcast, you will learn:
1. What is binge eating disorder?
2. What is food addiction?
3. What is emotional eating?
4. How do I know if I have binge eating disorder, food addiction or emotional eating.
Get a free copy of my book: “The Food Addiction Recovery Workbook” (I pay for the book, you pay for postage) – https://www.foodaddictionrecoveryworkbook.com/free?utm_source=crpodcast
If you’re an international listener use this link to get your free e-book of “The Food Addiction Recovery Workbook.” https://www.foodaddictionrecoveryworkbook.com/ebook
Schedule a free consult to discuss your food and body image issues: https://findingyouranchor.as.me/CONSULT
To learn more about The Anchor Program a 12-week non-diet program offering ONLINE group and individual sessions for the treatment of binge eating, emotional eating, food addiction and compulsive overeating. Want to learn more about the Anchor Program? https://AnchorProgram.com
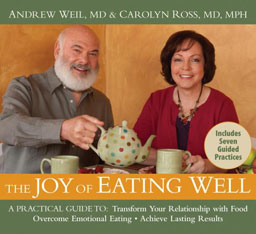
Hi, everybody. It’s Dr. Carolyn bringing you episode number 96 – What’s the difference between binge eating disorder, food addiction, and emotional eating. This is a common question that I get. So I’m going to bring you some patient examples as well as some definitions and how you can figure out if maybe you have one of those or an overlap of more than one, please stay tuned.
So the question again is what’s the difference between binge eating disorder, food addiction, and emotional eating. I want to illustrate some of these differences by telling you about previous patients of mine. And let’s start with Melinda. Who’s was a former patient who says “I eat and eat, and I know that I should stop, but I just can’t. I eat so much that I want to throw up and my stomach hurts and I have to lie down. Sometimes I feel like if I don’t eat everything, I can get my hands on. I’ll just explode.” Well, her words highlight the anguish that many people feel when food controls their lives. So Melinda often felt really powerless and out of control around food. And she also felt hopeless that her behavior could change. Her struggle with food is, is an example of what we’re going to talk about, about binge eating disorder, because that was her diagnosis.
So let’s start with some definitions and information about binge eating disorder. Well, first of all, up to 25% of people living in larger bodies who seek weight loss programs have actually have binge eating. And unlike other eating disorders, binge eating disorder appears to be almost as common in men has in women. So that’s unusual because for bulimia and anorexia, for example, it’s overwhelmingly women who struggled with that disorder. But for binge eating disorder, it’s almost as common in men as women. And it also affects African-Americans as often as Caucasians.
Now, if you have periods. And what you eat large quantities of food, more than what most people would eat in one sitting, you may have binge-eating disorder. Now, other symptoms include difficulty in controlling how much you eat and feeling powerless to stop eating, even though you may no longer be hungry or you may feel stuffed. Now, this isn’t just at Thanksgiving. I think all of us often have a little binge eating at Thanksgiving or other holidays, but this is something that would occur on a regular basis. Not specifically related to a holiday. After a binge, you may suffer from emotions of disgust and shame and embarrassment about how much you’re eating. You may eat in isolation because of embarrassment about how much you’ve eaten. For individuals who struggle with binge eating disorder, these behaviors around food, and also body dissatisfaction often began earlier than for their people. So they may have a history of dieting at a young age. I mean, I’ve had patients who’ve been put on diets at five years of age, which is unbelievable. And many times they’re told by the pediatrician your child needs to be on a diet. So they put them on a diet. The people I’ve seen are obsessed with body shape and size, and you know, they have a similar thought patterns about their body. As do people with bulimia. So individuals living in large, larger bodies is part of what makes it the criteria for binge eating disorder, but not everyone who has binge-eating disorder is living in a larger body. So we cannot judge it by the size or weight of a person it’s more determined by the behaviors. A hallmark of binge-eating disorder is interestingly a history of exposure to negative messages about shape eating and weight. Now while dieting maybe associated with binge eating disorder and many people bingeing behavior actually begins before dieting. But we do know that dieting will make, then she can disorder worst. Binge eating disorder is three times more common than anorexia and bulimia combined. And it’s the most common eating disorder in the United States in both, and it, and as I said, it occurs in both men and women almost secretly and it’s the most common eating disorder in adults in the United States. So you may be surprised by the statistic that it’s more common than anorexia and bulimia combined, because we hear so many, so much talk about those two eating disorders. And when you say eating disorders, in fact, most people think about anorexia and bulimia. They don’t think about binge-eating disorder, but binge-eating disorder is much, much more common.
So now let’s talk a little bit about addiction and here’s another patient who I’ve seen in the past. Her name was Jen and when we discussed her relationship with food, Jen became very animated. She was a self-described food addict, and she talked about how her heart rate would increase and our mouth would water when she was. Once she was even on the, in the car on the way to the grocery store. And particularly when she would walk down the chip aisle of the grocery store. She talked about trying to avoid even going shopping because she knew she wouldn’t be able to resist buying this large bag of chips that she described as her downfall. But she also described her anticipation of getting the chips and said it was a feeling like what she thought a drug addict would feel when they were going to score crack cocaine. She felt like a kid in a candy store guilt-free and excited about her purchase. And she sometimes felt the need to explain to the cashier why the bag was already open before she had even paid for it. And she would say things like, oh, I miss lunch today so I’m starving. She would make promises to herself and then bargains with herself to keep herself from buying the chips or is she gave into her craving she would promise herself she would eat just half the bag and then put them away. So she also came up with punishments that she would give herself if she slept. And so her eating felt completely out of control. So, how do you know if Jen had heard addiction or if you have food addiction? Well, there are no medical criteria for food addiction at this point. However, there’s a series of studies and then done using the Yale food addiction scale with a proposed list of criteria. And these are the same criteria that have been used to identify people with substance use disorders. So the Yale food addiction scale has found that 5 to 10% of the general population test positive on that Yale food addiction scale, including 7% of children who were tested. The Yale food addiction scale also shows that food addiction is 15 to 25% higher in those living in larger bodies compared to those normal weight by BMI, even higher rates include addiction are found in those who are seeking weight loss surgery or beriatrics surgery, or in those who are living in larger bodies and also have binge eating disorder. That incident is 30 to 50%.
So binge-eating disorder does share a number of characteristics with food addiction there is overlap. 57% of people diagnosed with PED, also meet criteria for food addiction and in both disorders, people experience the extreme lack of control over their eating and continued eating despite having negative consequences. Also the inability to change their behaviors, even though they really want to. Though there is that overlap between binge eating disorder and food addiction there are also differences. People with food addiction tend to experience even higher levels of poor self-esteem, depression and difficulty regulating their emotions. So one of the markers in the research on food addiction is that a hundred percent of those taking the test report the desire to cut back or stop their eating behaviors. So if you have food addiction, you’re likely to have more intense and frequent food cravings than someone without food addiction. And when people who have food addiction, see what we call highly palatable foods, or you can just call them comfort foods, their brains light up on scans in a way that’s different than those people without food addiction. And that this pattern is similar to the brain scans of people using drugs of abuse. But also doing any pleasurable activity, whether it be hugging your child, watching a sunset, you know, having a good dinner, et cetera. But if you are, if you have food addiction, you can, you may also be more likely to engage in emotional eating, which we’re going to talk about in just a moment.
So that’s food addiction, so we’ve talked about binge eating disorder. That’s eating a large quantity of food in one sitting, eating in isolation because of the embarrassment and feelings of emotional distress discussed, regret about how much you’ve eaten. Food addiction we’ve mentioned has some overlap with binge eating disorder, but also people with food addiction tend to have more intense food cravings. And have more extreme levels of feeling out of control and feeling emotional distress related to their eating.
So let’s talk now about emotional eating, emotional eating then can be defined as eating and response to emotional cues or eating to make yourself feel better or change your mood as it opposed to eating and response to being physical. So here’s one of my patients who has emotional eating disorder. Marianne just turned 60, she’s married. He has a successful career in nursing, although she feels good about most things in her life she continues to struggle with food and body image issues when she’s happy she overeats, when she sad or angry showrooms, when her husband has to work late and she’s home alone, she overeats. She describes food as best friend, even though she has read many guide books and has been on numerous fad diets, she can’t seem to stop herself from having a few more cookies. A few, always leads to half a bag or the whole bag. Then the guilt comes and she feels ashamed that having so little control. She really believes that if her life was less stressful, she could stop over eating or if her husband were more affectionate, she wouldn’t turn it for. So if, if you’re like many people with food and body image issues, you may be able to recognize that your emotions at times can feel overwhelming. And that is even if the emotion is “a positive emotion”, like feeling happy or having something to celebrate it doesn’t always have to be a negative emotion, but some people with emotional eating feel just flooded by any emotion and they then tend to either completely shut down or they may haveeal trouble, even naming what they’re feeling, naming the emotion. So both reactions to emotions are really flip sides of the same coin. When, when you’re stuck in what I call the emotional suit, you may feel that your emotions are in shock, in charge they’re in the driver’s seat and you’re in the backseat trying to reach forward and drive the car. So coming out of emerging from the emotional suit requires emotional development. And that is being able to identify express, be aware of, and regulate your emotions because it’s not your emotions. In other words, it’s not having an emotion that causes the problem. It’s really your inability to manage those emotions or it’s your attempts to avoid the emotions altogether. But when emotions are not acknowledged, they find expression in the foods that you eat in and also in the size and shape of your body and in the need to include that may be soothing for, you know, five minutes, but don’t quench the underlying root cause of your emotional eating.
So emotional regulation really means being able to learn the skills, to be able to cope with your emotions without always defaulting to food. So learning to identify your emotions, put a name on it, you know, they say in the 12 step programs, name it and claim it is the first step to being able to learn, to regulate your emotions in a healthy and safe way. And that’s important because it allows you to be the individual you are with your own perceptions and viewpoints. Emotional expression is a necessary part of what it means to be human. So let’s summarize. There is overlap between binge-eating disorder, emotional eating, food addiction. For example, you may binge, you may have food addiction and one of the behaviors you use is bingeing, or you may have binge eating disorder and any emotions may trigger a binge. So studies also show that dieting makes all of these disorders worse. so dieting isn’t the solution it actually is it can be a cause of the problem. The problem is also not with foods. So it’s food that’s the problem. It’s how you are using the food. In general food addiction causes more emotional distress and people are more obsessed about food then for those with binge-eating disorder or emotional eating. But for all three food is used to numb motions to tamp down on comfortable, even positive emotions, or to get back feeling in control when you’re experiencing negative emotions. For many people with binge eating disorder, emotional eating and food addiction, there is underlying childhood adversity or trauma or neglect. That was the beginning of them starting to use food in the way what they do also for most there’s there are associated body image issues, and sometimes there can be depression and anxiety.
Well, does it matter what the label is? Well, binge eating disorder is the only one of these disorders that is listed in the diagnostic and statistical manual of mental disorders and therefore the only one that may have some coverage under insurance. But beyond insurance covered coverage, I think the labels can help you have a better understanding of what’s going on with you and your relationship with food and your body. And it also helps you gets a name for what you’ve been feeling. This can make you feel like you’re not alone and offer you some sense of that what you’re experiencing is real. It’s not something you’ve made up. So, I think that’s one of the reasons why the label is helpful. But the bottom line is if you’re struggling, if you’ve been struggling for all your life, or even just recently with binge-eating disorder, food addiction, and emotional eating, there is help and support available.
As you know, I’ve written a book on each of these topics, and I also run The Anchor Program that is a non-diet approach to treating binge-eating disorder, emotional eating, and food addiction. The Anchor Program. We have one beginning very soon, so if you’re interested, please sign up for the free consult to see if you’d be a fit for the program and the link will be in the show notes. Also, I want to just remind you that I am offering a free copy of my book, The Food Addiction Recovery Workbook. You can get a free copy. You pay for the postage, how pay for the book and for our international listeners we’re now offering able to offer a free copy of the ebook for The Food Addiction Recovery Workbook. So just look in the show notes and you’ll see all the information you need to either find out about the anchor program and sign up for your free consult or get a free copy of The Food Addiction Recovery Workbook.
Okay. The next podcast we’ll we won’t be talking about healing from the, using the five levels of recovery and that’s healing from binge-eating disorder, food addiction, and emotional eating, using the five levels of recovery. And we’ll start with the first level, which is how you can stop unwanted behaviors. So please join us for the next podcast, please share, and give us a rating and share this podcast with anyone that you feel might benefit from it. Thank you for listening. This is Dr. Carolyn signing off.
So thanks for listening to the show. I hope that clarifies the distinctions between binge eating disorder, food addiction, and emotional eating for you. And I hope that if you are struggling with one of those that you reach out for help, whether it be to, if you have food addiction, there are certainly 12 step programs that are available through food addiction recovery anonymous, you can get a free copy of my book, the food addiction recovery workbook, also the emotional of not offering free copies, but you can purchase the emotional eating workbook or the binge eating disorder and compulsive reading workbook. Those are all available on my website and you’ll see all those links in the show notes. Please give us a rating. I hope you’ll give us five stars and again, share the podcast. Help us get the word out about binge-eating disorder, food addiction, and emotional eating. Appreciate you. And I’ll see you next time. When we be talking about that first level of healing from binge eating disorder, emotional eating or food addiction, which is the superficial level of behaviors and how we can stop unwanted behavior such as binge eating, cravings obsessing about food and so on. So that’s going to be our plan for the next five podcasts. We’re going to be diving into the exact ways I work with clients in the anchor program to take them through the five levels of recovery. So don’t miss even a one. Be sure you stay tuned for the next one.
All right. Thank you for listening. See you next time.